Carpal tunnel syndrome is a common condition that causes pain, numbness, and tingling in the hand and forearm.
The condition occurs when one of the major nerves to the hand — the median nerve — is squeezed or compressed as it travels through the wrist.
Surgical treatment for carpal tunnel syndrome is relatively simple and patients generally get very satisfying results.
Carpal tunnel syndrome often gets worse over time, so early diagnosis and treatment are important. Early on, symptoms can often be relieved with simple measures like wearing a wrist splint or avoiding certain activities.
If pressure on the median nerve continues, however, it can lead to nerve damage and worsening symptoms. To prevent permanent damage, surgery to take pressure off the median nerve may be recommended.

Anatomy
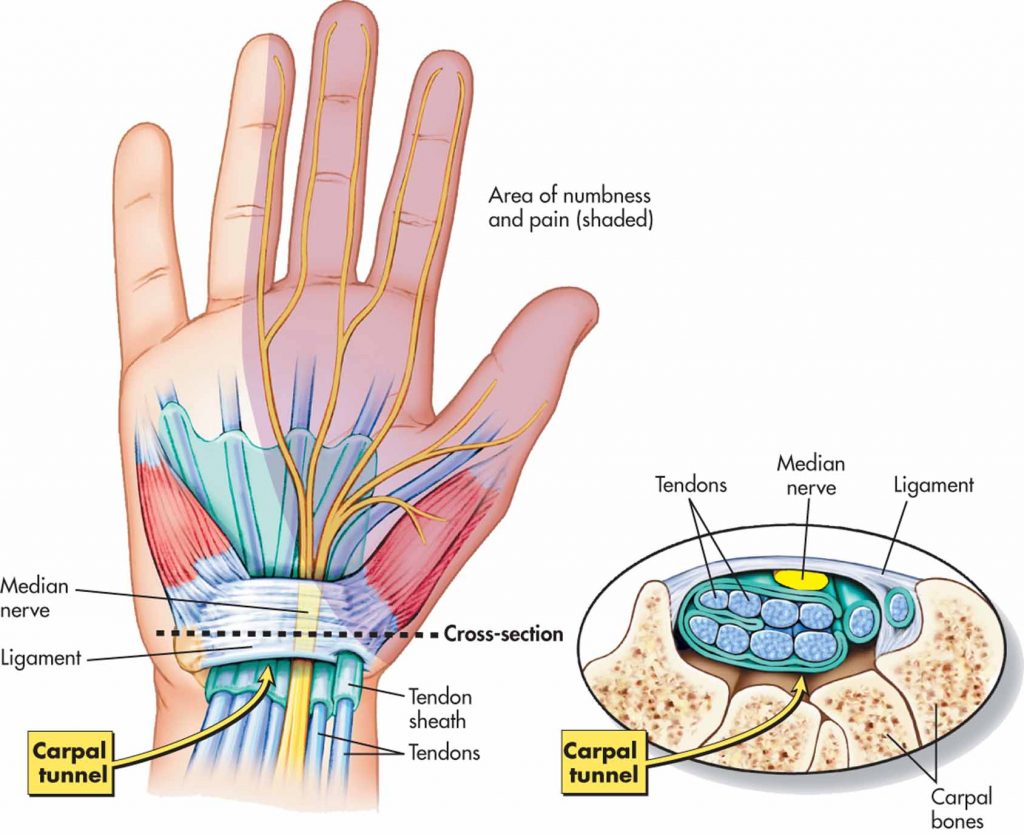
The structures forming the boundaries of the carpal tunnel are the carpal bones and the transverse carpal ligament. The contents of the carpal tunnel include the median nerve, the flexor tendons of the hand and the tissues surrounding the tendons (tenosynovium).
The space for the median nerve in the carpal tunnel may therefore be reduced by arthritis and other issues with the bones and joints of the wrist or thickening of the tendons or tenosynovium passing through the tunnel.
Certain postures of the wrist will also result in more pressure on the median nerve.
The median nerve originates from nerve roots in the neck. The nerve develops from branches of a network of nerves known as the brachial plexus then passes down the arm and forearm to the hand. It supplies skin and muscles in the forearm and hand. It specifically supplies the palmar skin of the thumb, index and middle fingers. It supplies the muscles at the base of the thumb.
Causes
Carpal tunnel syndrome (CTS) is very common. It is however more common in women and older people. Inherited factors that produce a small tunnel will increase the risk of CTS. Some positions of the hand which involve wrist flexion for a prolonged period (driving, reading, use of the telephone increase pressure on the nerve. Repetitive hand actions may result in swelling of the tendons and tenosynovium passing through the tunnel. Pregnancy causes generalized fluid retention. Carpal tunnel syndrome in pregnancy is very common. Certain medical conditions like rheumatoid arthritis, diabetes and thyroid disease are also associated with carpal tunnel syndrome.
Symptoms
The symptoms of carpal tunnel syndrome include numbness and tingling in the digits of the hand. Typically the symptoms are worse at night and can disturb sleep. Pain or electric shock like symptoms can be experienced in the hand or up the forearm. On rare occasions discomfort may radiate up the upper arm.
Difficulty with fine movements such as doing up buttons may be affected by numbness and weakness of the thumb. Dropping objects such as coffee cups can also occur due to weakness and numbness.
Examination
Dr Hutabarat will look for wasting of the thenar muscles at the base of the thumb and numbness in the thumb, index and middle fingers. Tinel’s test (tapping on the nerve) and Phalen’s test (flexion of the wrist) also may cause some symptoms.
Laboratory tests like nerve conduction tests and EMGs may help to determine if other causes of numbness like peripheral neuropathy are present.
An XR may show arthritis of the carpal bones and an MRI may be useful if other lesions in the wrist are suspected.
Treatment
Treatment varies depending upon the cause of the CTS. If the cause is temporary like pregnancy a temporary solution like a splint may be all that is required. If the cause is a temporary flare of rheumatoid disease an injection and modification of rheumatoid medications may settle the symptoms.
Medications like non-steroidal anti-inflammatories may decrease pain. Modification of activities to avoid aggravating factors, if this is possible, may be all that is required.
Longstanding carpal tunnel syndrome will result in permanent weakness and a delay in recovery of sensation. Prompt surgical treatment may therefore be preferred in most cases.
There are two surgical operations:
- Open carpal tunnel release
- Endoscopic carpal tunnel release
Open carpal tunnel release gives good access to the structures in the tunnel and enables visualization of other pathologies that may be involved. Endoscopic release avoids a scar in the palm but does not allow for other structures to be examined. A slightly higher risk of damage to nerves in the hand has also been reported.
At the end of the procedure the tissues are infiltrated with local anaesthetic which will make the wound and the hand numb for a number of hours. The wounds are closed with a horizontal mattress suture that makes the skin edges sit up.
Recovery
After surgery, you will be moved to the recovery room and should be able to go home within 1 or 2 hours. Be sure to have someone with you to drive you home and check on you that first evening. While recovery from knee arthroscopy is faster than recovery from traditional open knee surgery, it is important to follow your instructions carefully after you return home.
Have a question or inquiry or looking for some more information about our services, get in touch and we will be happy to assist.