This information will help you understand the pros and cons of total hip replacement.
We will look at how a normal hip works, causes of hip pain and what to expect from hip replacement surgery. There are certain exercises and activities that will help restore your mobility and strength postoperatively and will help you to return to everyday activities.
The most common cause of hip pain is osteoarthritis. A hip replacement may also be required after a fracture, or other conditions like rheumatoid arthritis. Hip arthritis will make activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff, and it may be hard to put on your shoes and socks. You may even feel uncomfortable while sleeping. It is not uncommon for hip arthritis pain to be felt as pain radiating into the groin or down the thigh to the knee.
If non-surgical means such as medications, activity modification and a stick or crutches do not adequately help your symptoms, you may consider hip replacement surgery. Hip replacement surgery is a safe and effective procedure that can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
Hip replacement surgery was pioneered by John Charnley in the 1960’s. It remain one of the most successful operations of all time. Since its inception there have been many improvements in hip replacement surgical techniques and technology. More than 50,000 total hip replacements are done each year in Australia.
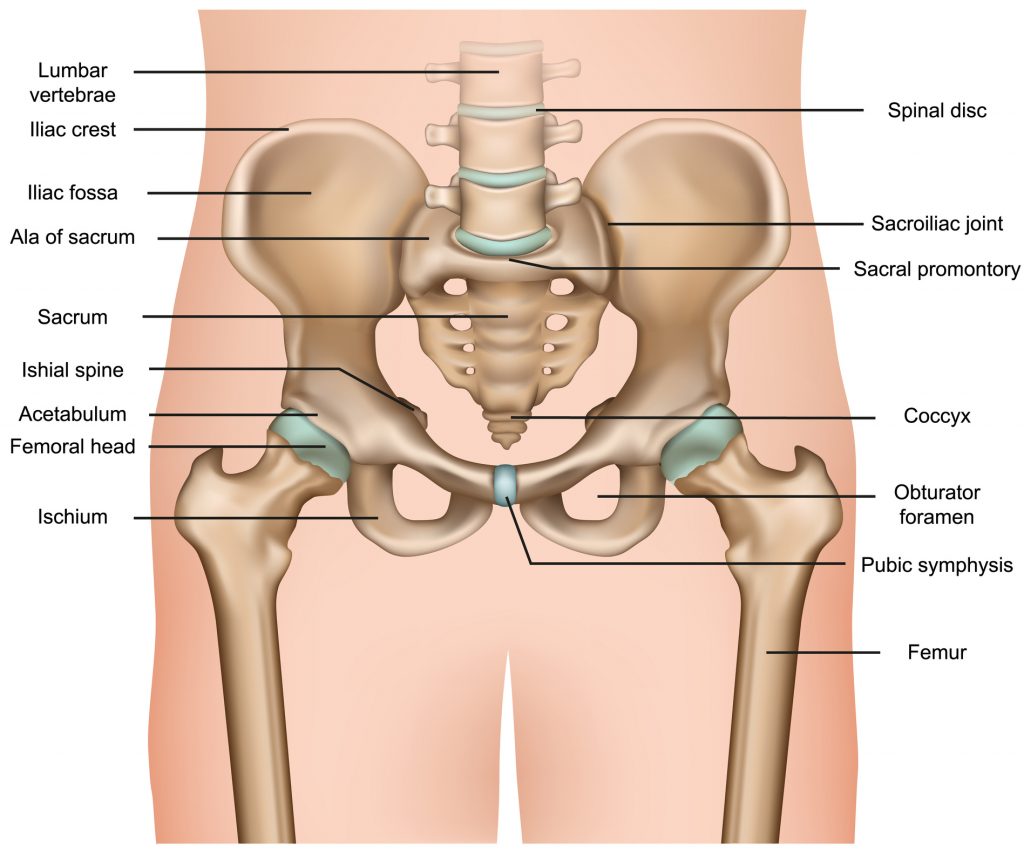
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the pelvis. The ball is the femoral head, which is the upper end of the thigh bone.
The bone surfaces of the ball and socket are covered with articular cartilage which is smooth and lubricated by fluid produced by the synovium. This enables the joint to move easily. Ligaments connect the ball to the socket and provide stability to the joint.
Common Causes of Hip Pain
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
-
Osteoarthritis
This is an age-related “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones of the hip wears away much like the tread on a tyre will wear with time and use. The bones then rub against each other, causing hip pain and stiffness.
Osteoarthritis may also be caused or accelerated by subtle irregularities in how the hip developed in childhood.
-
Rheumatoid arthritis
This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. Chronic inflammatory products can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed “inflammatory arthritis.” Psoriatic arthritis is another form of inflammatory arthritis.
-
Post-traumatic arthritis
This can occur after a fracture or dislocation. The cartilage may become damaged and lead to hip pain and stiffness over time.
-
Labral pathology and FAI
Sometimes soft tissue injuries such as labral tears can result in premature development of osteoarthritis. A pathology called femoro-acetabulur impingement (FAI) can also lead to premature arthritis of the hip joint.
-
Avascular necrosis
A dislocation or fracture, may limit the blood supply to the femoral head. This may also occur with certain drugs. The decreased blood supply may cause the bone cells to die. Over time the bone may collapse with resulting arthritis. Some diseases can also cause avascular necrosis.
-
Childhood hip disease
Hip disease or developmental changes in infants and children can lead to early arthritis.
The Procedure
Planning
Planning is a vital step in ensuring that hip replacement surgery achieves the best possible result.
Traditional planning involved holding plastic templates up against x-rays that are placed on a viewing box. More modern techniques involve CT planning that enables 3-D reconstruction of bones and implants with re-construction of the centre of rotation of the joint. Modern CT planning allows for better management of complex abnormalities. Custom made 3-D printed jigs can be used to optimise cuts and positioning. They can be made to fit laser guidance systems that can optimise positioning also. In the rare circumstances of significant anatomical abnormalities, custom made implants can be produced.
Approaches
In a total hip replacement damaged bone and cartilage is removed and replaced with prosthetic components.
The path a surgeon takes into the body is known as the approach. The three main approaches used for hip replacement are the anterior, posterior and anterolateral approaches. Each of them have different pros and cons.
-
The anterior approach
The anterior approach is a safe approach that has the advantage of a more comfortable initial postoperative course and a lower dislocation rate. This is balanced against a slightly higher fracture risk and a steeper learning curve for the surgeon. Technology over the past 15 years has improved the use of this approach which has actually been around since the early days of hip surgery in the 1930s.
-
The posterior approach
The posterior approach is probably still the most commonly used approach for hip surgery. It gives a good view of the pathology and allow exploration of the sciatic nerve if this is required. It is the most common approach used for revision surgery as it can be extended further up and down the limb if required.
-
The anterolateral approach
The anterolateral approach is commonly used for fractures of the sub-capital region of the hip. It has a low dislocation rate but patient will have a limp for months after.
Dr Hutabarat will weigh up the pros and cons of the approach the best suits your situation. Feel free to discuss this at your consultation.
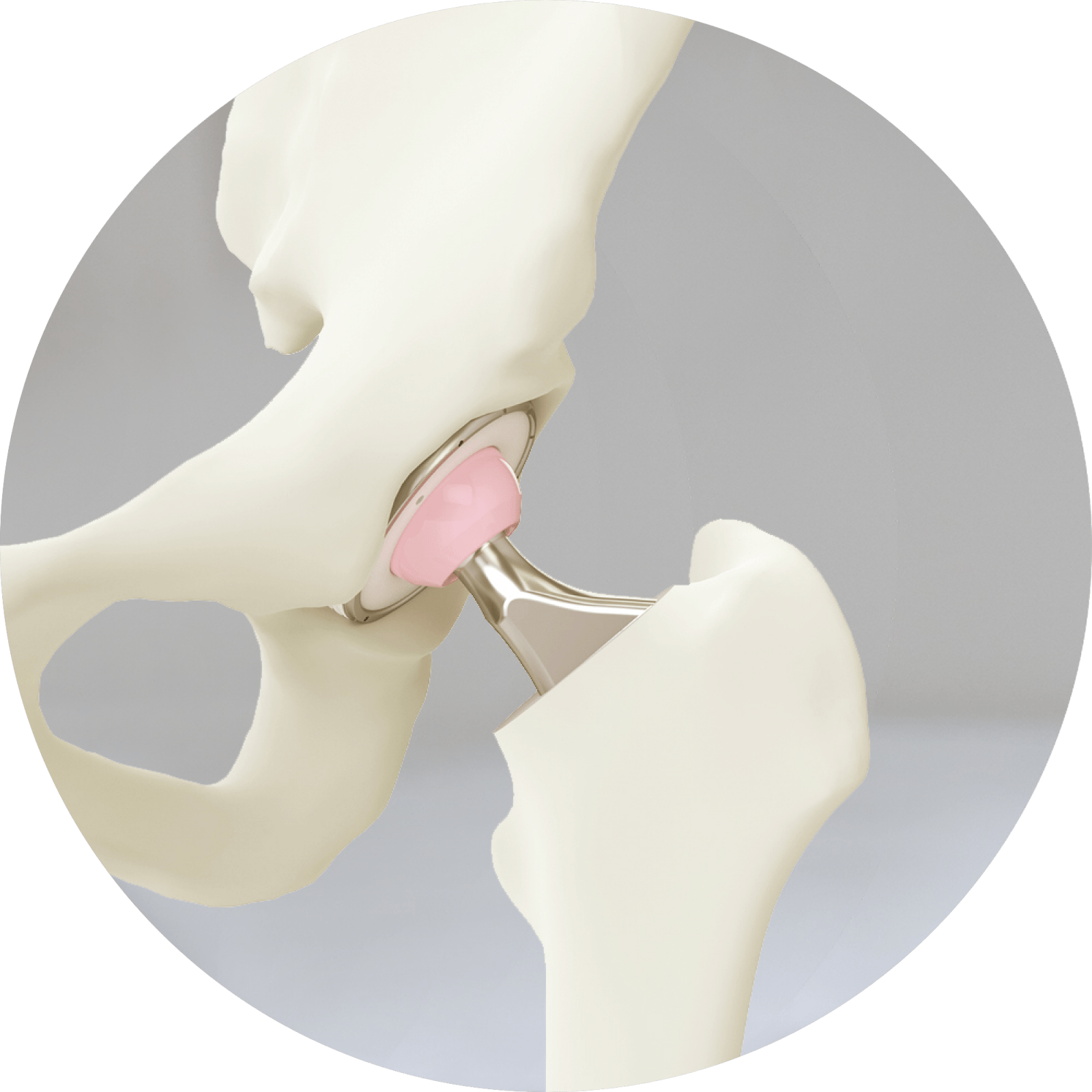
Implantation
The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow centre of the femur. The femoral stem may be either cemented or “press fit” into the bone. A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the damaged femoral head that was removed.
The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place. Special coatings may be used on press fit implants to encourage bone to grow onto and integrate the implant. A plastic or ceramic spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements. It is recognised however that complication rates and satisfaction rates improve significantly with patients who have a BMI less than 30.
Recommendations for surgery are based on a patient’s pain and disability, not age. Most patients who undergo total hip replacement are age 50 to 80, but orthopaedic surgeons evaluate patients individually. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
When Surgery Is Recommended
There are several reasons why you may be recommended hip replacement surgery. People who benefit from hip replacement surgery often have:
- Hip pain that limits everyday activities, such as walking or bending
- Hip pain that continues while resting, either day or night
- Stiffness in a hip that limits the ability to move or lift the leg
- Inadequate pain relief from anti-inflammatory drugs, physical therapy, or walking supports
The Orthopaedic Evaluation
An orthopaedic evaluation consists of several components.
- Medical history. We will gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform everyday activities.
- Physical examination. This will assess hip mobility, strength, and alignment.
- X-rays. These images help to determine the extent of damage or deformity in your hip.
- Other tests. Occasionally other tests, such as a magnetic resonance imaging (MRI) scan, may be needed to determine the condition of the bone and soft tissues of your hip.
Deciding to Have Hip Replacement Surgery
Talk With Dr Hutabarat
Dr Hutabarat will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options — such as medications, physical therapy, or other types of surgery — also may be considered.
In addition, Dr Hutabarat will explain the potential risks and complications of hip replacement surgery, including those related to the surgery itself and those that can occur over time after surgery.
Never hesitate to ask questions when you do not understand. The more you know, the better you will be able to manage the changes that hip replacement surgery will make in your life.
Realistic Expectations
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and cannot do. Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living.
With normal use and activity, the material between the head and the socket of every hip replacement implant begins to wear. Excessive activity or being overweight may speed up this normal wear and cause the hip replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports.
Realistic activities following total hip replacement include unlimited walking, swimming, golf, driving, hiking, biking, dancing, and other low-impact sports.
With appropriate activity modification, hip replacements can last for many years.
Preparing for Surgery
-
Medical Evaluation
If you decide to have hip replacement surgery, Dr Hutabarat may ask you to have a complete physical examination by your GP before your surgical procedure. This is needed to make sure you are healthy enough to have the surgery and complete the recovery process. Many patients with chronic medical conditions, like heart disease, may also be evaluated by a specialist, such a cardiologist, before the surgery.
-
Tests
Several tests, such as blood and urine samples, an electrocardiogram (ECG), and chest x-rays, may be needed to help plan your surgery.
-
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact the hospital or the rooms for treatment to improve your skin before surgery.
If you have particularly dry flaky skin it may be an idea to moisturise it to improve its condition in the weeks prior to surgery. Organisms live on our skin. We do not want them floating around the operating room on tiny flakes of your dry flaky skin.
-
Blood Management
You may be advised to improve your ability to produce blood cells prior to surgery. This can be done several ways. If you are not able to have blood products for any reason please inform Dr Hutabarat.
-
Medications
Tell the practice about the medications you are taking. The practice or the preadmission clinic staff will advise you which medications you should stop taking and which you can continue to take before surgery.
-
Weight Loss
If you are overweight, you may be asked to lose some weight before surgery to minimise the stress on your new hip and possibly decrease the risks of surgery.
-
Dental Evaluation
Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your hip replacement surgery.
-
Urinary Evaluation
Individuals with a history of recent or frequent urinary infections should have a urological evaluation before surgery. Older men with prostate disease should consider completing required treatment before having surgery.
-
Specialised Geriatric Assessment
Some elderly people may require specialised geriatric assessment preoperatively or postoperatively. If you think either yourself or your relative may benefit from this, please notify Dr Hutabarat’s staff. There are several geriatricians and rehabilitation experts at the facilities at which surgery or recovery may take place. The practice has considerable experience in managing these issues and Dr Hutabarat has given many talks on a national level regarding orthopaedic management of elderly patients.
-
Social Planning
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone, a discharge planner or the rehabilitation team at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in a rehab facility during your recovery after surgery also may be arranged.
-
Home Planning
Several modifications can make your home easier to navigate during your recovery. These are more likely to be required in the very frail patient who is still in rehab postop. A discharge planner and a home visit prior to discharge may be used to determine what is required. The following items may help with daily activities:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
- Tongs or a reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
Have a question or inquiry or looking for some more information about our services, get in touch and we will be happy to assist.